The Intelligent Spine Interface
Restoring sensorimotor function through epidural electrical stimulation.
Following a complete spinal cord injury (SCI), the descending motor commands from the brain can no longer reach their target musculature. Additionally, ascending sensory signals from the periphery cannot pass through the injury site to reach the brain for interpretation. As a result, there is significant sensorimotor deficits below the level of injury.
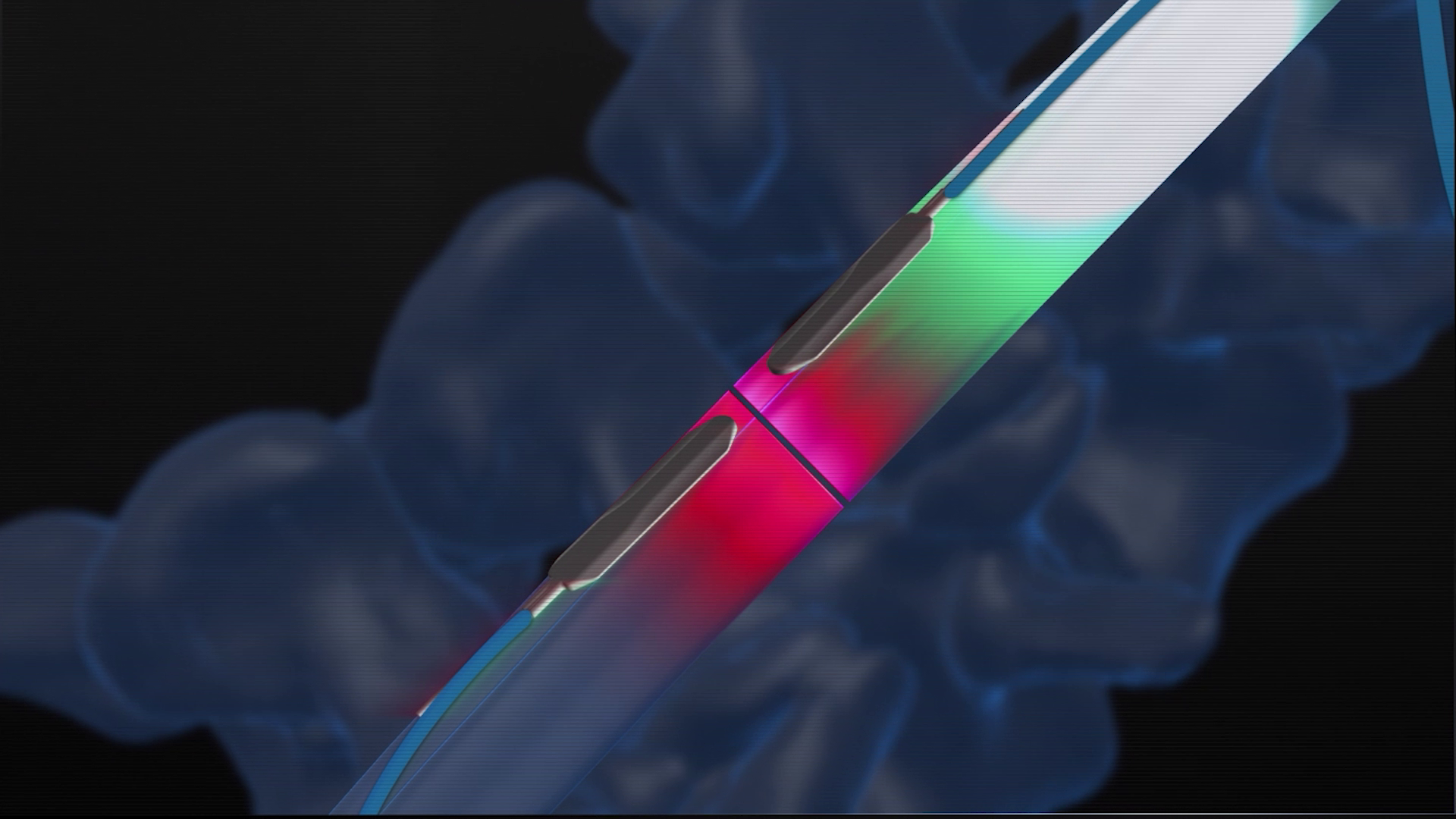
To understand how the signals in the spinal cord are affected, and how we can modulate these signals to restore function following an injury, I am working on the Intelligent Spine Interface project. This project uses a novel, two-electrode system to simultaneously stimulation and record from the spine both above and below the level of injury.
Developing useful sensory neuroprostheses.
While I have played a key role in many aspects in the preclinical and clinical studies, my research particularly focuses on the restoration of sensory function in humans through epidural electrical stimulation (EES). While there has been significant recent success in restoring motor function using EES, sensory function has been neglected. It is well known that the inclusion of sensory feedback during the use of a prosthetic can greatly improve motor control and coordination, so including sensory feedback during EES-based motor restoration may net additional performance improvements. How we interpret sensory information is highly personal, and can be influenced by a multitude of bottom-up (e.g. intensity, temporal application) and top-down (e.g. attentional) factors. When we provide sensory feedback, in order for the feedback to be useful we need to calibrate the feedback to the interpretation of the user. My work serves as an initial investigation into the dependence of stimulus detectability and discriminability on changes in high-dimensional stimulation parameters.

A lens for translation.
One of the things that excites me most for the EES-based sensorimotor restoration is the proximity of translation. The electrode paddles and implantation techniques are the same used in tens of thousands of surgeries per year in the U.S. for neuropathic pain, so surgeons and regulatory agencies are familiar with the technology. To move towards a take-home study, I have developed novel participant-in-the-loop control interfaces, giving control of sensory restorative stimulation to the participants. I hope that these interfaces will improve the accessibility of future sensory neuroprosthetic devices, as day-to-day or positional changes in stimulation interpretation can be adjusted without expert intervention.